Europe
RefluxStop™ is CE marked in Europe. It is currently available in:
- Germany
- United Kingdom
- Switzerland
- Spain
- Italy
- France
- Austria
- Sweden
- Norway
Prioritized Products
Urology
Implantica’s UriControl® is subject to further development and approval process.
UriControl® is designed to have the ability to significantly improve on existing manual pump concepts to treat urinary incontinence with the use of Implantica’s innovative wireless energized technology and Smart device design.
Most importantly, UriControl’s design goal is to also address the 10% of all women suffering from urinary leakage where no optimal treatment exists today.1
UriControl® is designed with smart medical implant functionality.
The principle of UriControl® is well proven as the hand pumped artificial urinary sphincter device exists on the market today. UriControl® is expected to be both more convenient and hygienic to use as well as offering improved treatment functionality since it is designed to be operated by a remote-control or push button under the skin. UriControl® is a smart active implant with an advanced pressure regulation system which will work directly on the urethra. It is estimated to both reduce complications and improve treatment efficiency.
UriControl® has the potential to also address the much-underserved female market.
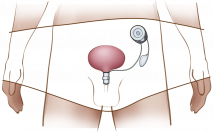
UriControl® is targeted to become a device to treat urinary incontinence for both men and women, designed to be recharged wirelessly, it has the potential to radically improve quality of life for a very large number of people by providing a solution that restores their dignity and freedom.
Urinary treatment device market:*
200m – Number of global sufferers1-3
10% – Of all adult women1,2
20% – Of all prostate cancer operated men1,3
Valued at USD 3.1 billion 2023
CAGR 9% forecasted 2024 - 2032
Forecasted USD 6.1 billion 2032
UriControl® is designed to eliminate the need for manual pumping and allow the bladder to be emptied on demand through a user-friendly and convenient interface, controlled by a remote control.
UriControl® is anticipated to also be available for women, with the potential to fill a large market need in the magnitude of 500’000 procedures p.a.2
The UriControl® system is planned to provide different pressure at different times according to the need, which should improve both functionality and safety. Existing treatment with a hand pumped device needs to maintain a constant low pressure to avoid damaging the urethra.
The existing hand pumped device, created by other manufacturers, has been on the market for 20 years and is a strong proof of concept.
Voiding dysfunction is a disruption in the ability to urinate or in the ability to consciously control the urination process leading either to urinary incontinence or urinary retention.
Implantica is focusing on treatment for both urinary retention and urinary incontinence.
Urinary incontinence is a common and often embarrassing problem, which can have a very negative impact on a sufferer’s quality of life. It may affect both young and old, although often surfaces later in life and is common in women, affecting 10% of all women. It has many different causes including the physical strain of childbirth, low estrogen levels after menopause and, for men, side effects related to prostate surgery. Urinary incontinence can have a profound impact on the sufferer’s self-esteem and sense of dignity.
Additional treatment solutions in this field such as urinary retention, are part of our pipeline.
No optimal treatment exists for urinary incontinence. The most commonly used surgical and implanted treatment methods for severe stress incontinence and intrinsic sphincter deficiency are described below.
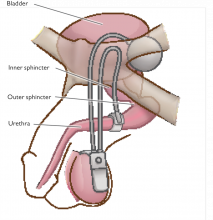
Artificial urinary sphincter (AUS). This is the primary treatment solution for men, which uses a silicone cuff or similar device to compress the urethra in order to close it, mimicking a biological sphincter muscle (see Figure 2). This hand pumped device is controlled by a manually manipulated pump placed in the scrotum (as a third testicle) or in the area of labia majora. While the device works well as intended, the hand-pump can be burdensome at times as the tissue may become irritated and painful to squeeze with repetitive use. This implant is quite rarely used for women due to the more complicated surgical procedure, a lack of space to place the hand-pumped device as well as the discomfort for female patients of manipulating a pump placed in the labia.
The manually manipulated pump has shown success rates of up to 94% (Barry, 2003). The most common indication for AUS placement is male stress urinary incontinence due to radical prostatectomy (RP), so-called post-prostatectomy incontinence. Today there are two commercially available AUS, American Medical Systems’ AMS 800 and Zephyr.
Sling procedures. For women, the most common procedure is a sling placed under the neck of the urinary bladder to try to lift the position of the urinary sphincter and prevent it from descending during physical activity, which indirectly improves urinary leakage. Mesh is also used to lift both the neck of the bladder and a fallen uterus. These procedures are the main surgical methods for treating female stress incontinence. Success rates are in the region of 85% but may be less in the long-term (Barry, 2003). The only available figures on the number of surgeries have shown about 500’000 surgeries performed p.a.3, however, complications exist with so-called migration/erosion, where the sling and mesh pass through tissue, and litigation against these methods constrain the market.
Transvaginal tape. Tension-free transvaginal tape (TVT) works in a similar way to a sling, but instead of supporting the bladder neck, the tape is placed around the mid-section of the urethra. TVT has fairly high success rates but can cause more erosion due to its mid-urethral placement, which is a serious side-effect. TVT is used for treating female incontinence. Success rates in the region of 60-70% have been reported (Barry, 2003).
Bulking material implants. Bulking agents such as collagen, silicone or carbon can be injected into the tissues surrounding the bladder neck for improved support and to aid the closure of the urethra in cases of stress incontinence caused by sphincter deficiency. Symptomatic relief is achieved in around 30-50% of women undergoing bulking implant procedures but is relatively short-term and usually require multiple injections (Barry, 2003).
Electrical stimulation. Electrical stimulation of nerves and muscles has proven to be successful for treating certain cases of stress incontinence and urge incontinence. In these cases, usually either the pelvic floor muscles or the sacral and posterior nerves have been subjected to electrical stimulation. A commonly used product for nerve stimulation for incontinence treatments is the Medtronic InterStim® Therapy.
Urination, also known as micturition or voiding, is the process of disposing urine from the urinary bladder through the urethra to the outside of the body. Urinary dysfunction refers to disruptions in the ability to urinate or in the ability to deliberately control the micturition process, normally described as urinary incontinence or urinary retention. Having voiding problems will unconditionally have a negative impact on a sufferer’s ability to work, their social life and day-to-day activities. Implantica is developing a product for the treatment of urinary incontinence, using new wireless technology and remote-controlled implants, targeted to present patients with a convenient and sustainable improvement of their quality of life.
Overview
Urinary incontinence is the loss of bladder control resulting in a varying degree of uncontrollable urine leakage. Although the condition itself is benign (not a serious health threat), it is usually associated with embarrassment due to its social consequences. Having problems with urinary incontinence is very common, especially among elderly women or men following prostatectomy (removal of the prostate). Problems with incontinence may often be a serious hindrance in day-to-day activities, and constantly being restricted by the risk of visible soiling or the adjacency to a toilet may greatly affect peoples’ quality of life.
Causes and effects
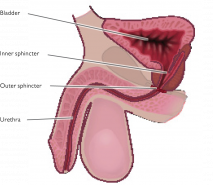
The most common type of incontinence is called stress urinary incontinence (SUI); leakage of urine when pressure is put on the bladder. This can happen during sports, when laughing or coughing or doing other physical activities. It is caused by a weakened sphincter muscle (see Figure 1) or weakened pelvic floor muscles. For women, possible causes to SUI include changes in hormone (oestrogen) levels and nerve functions from aging, pregnancy and menopause. For men the most common cause is complications related to prostate surgery.
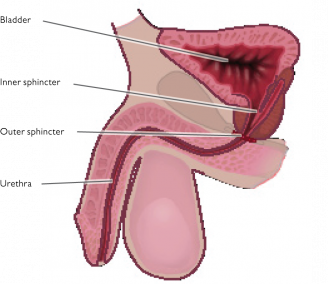
Fig.1
The second most common type of incontinence is urge incontinence. Urge incontinence is characterized by a sudden and strong urge to urinate that is hard to suppress. The urge is often intense enough to be followed by an unintended loss of urine. A more familiar expression for the condition is “overactive bladder”. The symptoms of overactive bladder occur in most cases because the muscles of the bladder involuntarily and prematurely contract. With normal bladder function this is supposed to happen voluntarily when voiding, in coordination with relaxation of the pelvic floor muscles and the urinary sphincter muscles. The causes of an individual patient’s involuntary bladder contractions are hard to identify, but common reasons are neurological disorders (such as Parkinson’s disease or due to spinal cord injury), urinary tract infection, abnormalities in the bladder (such as tumours), enlarged prostate, constipation or previous incontinence surgery.
Problems with voiding dysfunction are a large economic burden on society. For example, the cost of urinary incontinence in the US is estimated to be approximately USD 16.3 billion every year, counting costs of routine care, nursing home admissions, treatments, associated complications as well as diagnosis and evaluations (Wilson et al., 2001).
The largest portion of the direct economic burden of voiding dysfunctions comes from routine care. In the case of incontinent American women, routine care stood for 70% of the total incontinence costs, while the total cost of all treatment (surgical as well as pharmaceutical) was less than 10% of the incontinence-related expenditures (Wilson et al., 2001). This indicates that safe, sustainable and life-long treatments such as the implant being developed by Implantica could radically reduce the costs of routine care and lead to a more cost-efficient treatment of voiding disorders.
Having problems with the urinary cycle may be a serious hindrance in day-to-day activities, leave the patient with a considerably decreased sense of freedom as well as, in some cases, become a serious health threat if left untreated. Implantica is developing a solution to patients with severe voiding dysfunction, whether it is post-prostatectomy incontinence or female incontinence. Implantica’s device aims to offer a previously unavailable restoration of a patient’s quality of life due to remote controlled devices energized wirelessly, and ground-breaking stimulation technology combined with hydraulic constriction.