Europe
RefluxStop™ is CE marked in Europe. It is currently available in:
- Germany
- United Kingdom
- Switzerland
- Spain
- Italy
- France
- Austria
- Sweden
- Norway
Follow-on Products
Gastrointestinal
Implantica’s RectalRestore® is subject to further development and approval process. RectalRestore® is being designed to be our innovative solution to the debilitating impairment of anal incontinence. Our wirelessly controlled and rechargeable implant is being designed to manage defecation for patients suffering from fecal incontinence, an often embarrassing and isolating condition. As an active sphincter implant, RectalRestore® will be based on similar functionality and technology as UriControl®, our potential solution to urinary incontinence.

RectalRestore® is being designed to have the potential to allow patients complete control over their bowel emptying by a combination of applied hydraulic pressure and electrical stimulation onto the intestine. The solution could potentially enable opening and closing of the bowel in a manner that mimics the bowel organs’ natural functions.
RectalRestore® could potentially enable opening and closing of the bowel in a manner that mimics the bowel organs’ natural functions.
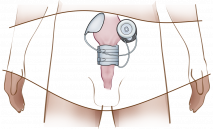
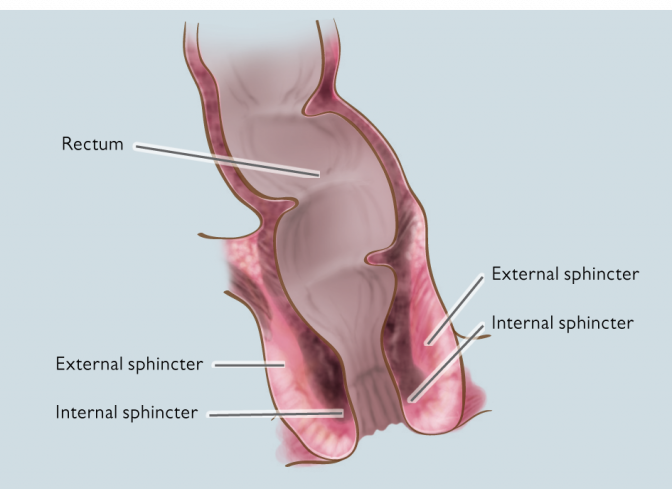
RectalRestore® is being designed to have a wirelessly adjustable hydraulic cuff that is intended to apply a minimum of force against the anal canal, and electrical stimulation should then close the remaining opening completely. By regularly changing the position of the electrical stimulation, steady blood circulation in the intestinal wall is estimated to be achieved, with the intention to prevent erosion or any other damage to the bowel, which could be a significant improvement over existing treatment procedures. The implant is planned to be placed in the body through laparoscopy which could minimize infection risk significantly as compared to existing solutions.
Implantica’s RectalRestore® is subject to further development and approval process and is not yet on the market. The easily adjustable remote control is designed to enable patients with fecal incontinence to control bowel movements, thereby intended to improve patients’ quality of life and social confidence.
RectalRestore® is designed with adaptable intelligent closure intended to prevent damage to the bowel. The closing mechanism is expected to be controlled not only by hydraulic pressure but also by electrically evoked physiological contractions, constantly changing position.
Existing treatment solutions have very high incidence of infection. Risk of infection could be drastically reduced since RectalRestore® is placed laparoscopically via the abdomen rather than with open surgery from the anus region.
Fecal incontinence (FI) is the inability to control bowel movements causing the unintentional passage of feces or stool from the rectum. The symptoms can range from an occasional leakage of stool while passing gas to a complete loss of bowel control. The International Foundation for Functional Gastrointestinal Disorders (IFFGD) defines fecal incontinence as “the involuntary loss of solid or liquid stool sufficient enough to result in impaired quality of life for the individual”.
FI is surprisingly common and affects men and women of all ages but is most frequent among older people. It is approximately twice as prevalent among women as men, as the condition may result from childbirth or obstetric trauma when injury to the anal sphincter muscle can occur. It affects more than 2 – 10% of the world population1 or 195 million people, based on an assumption of 3% of the total world population. Underlying causes include inflammatory bowel disease, intra-abdominal infection, injury to the anal sphincter or colorectal cancer, which is one of the most common types of cancer.
FI is a major burden to both patients and society. It can be socially devastating and has a significant impact on the patients’ freedom of action and movement. Patients often feel ashamed and embarrassed, and fear of public humiliation may lead to social isolation. The affected person often tries to hide the problem. Although most common in elderly people in residential care this disease is common also in people of younger age, for example childbirth is a common cause for incontinence among younger women.
No optimal treatment method for fecal incontinence exists on the market today with current treatments often not successful and complications with infections after surgery common. The need for surgery with up to 195 million sufferers is large, however, no optimal treatment exists and therefore only a small number of surgeries are performed.
Sphincter repair is the standard procedure which is performed on patients with a dysfunctional rectal sphincter due to injury, most commonly during childbirth, or aging. The procedure consists of re-attachment of the rectal muscles to tighten the sphincter and increase the strength of the anus. Treatment success with this procedure deteriorates over time, with only approximately half of the patients remaining continent after 3 years.4
Dynamic graciloplasty is a procedure for those with severe FI and involves a muscle transposition of the gracilis muscle, from the inner thigh, around the anal sphincter to restore bowel control. The procedure can initially be successful, but function deteriorates quickly due to muscle wastage and inability to maintain prolonged muscle contraction.
Sacral nerve stimulation involves application of electrical energy in the abdomen by using an implanted electronic pulse generator to achieve continuous muscle stimulation. The pulse generator is deactivated when the patient wishes to affect defecation. This method never achieved any success as other functional nerves need to be cut.
An artificial bowel sphincter is implanted for end-stage FI patients after other treatments have failed. This surgery is associated with high morbidity and common adverse effects include infections and device erosion5 with almost 50% of patients requiring revision surgery.6
When success is not achieved from other treatment methods, the end alternative is ostomy surgery. An ostomy is a procedure creating an opening in the body for the discharge of waste, which can be temporary or permanent.
Fecal incontinence (FI) – the loss of bowel control – affects about 120 million men and women around the world. For large numbers of patients with severe FI, the end treatment is ostomy surgery.
Fecal incontinence (also referred to as bowel incontinence or stool incontinence) involves the inability to control bowel movements. The symptoms can range from an occasional leakage of stool while passing gas, to a complete loss of bowel control. The International Foundation for Functional Gastrointestinal Disorders (IFFGD) defines fecal incontinence as “the involuntary loss of solid or liquid stool sufficient enough to result in impaired quality of life for the individual”.
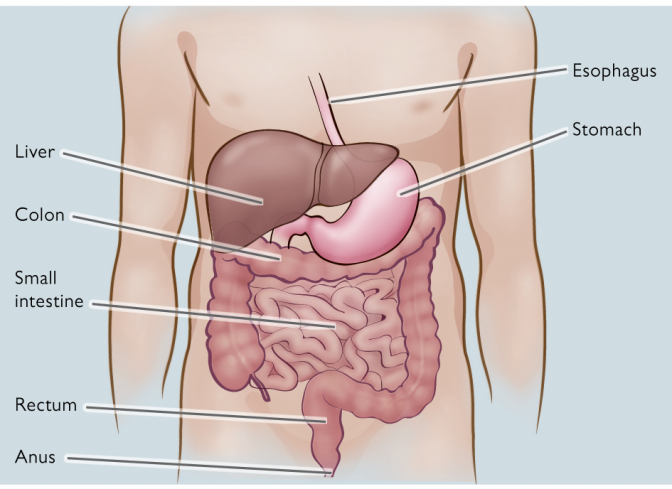
The intestines extend from the stomach to the anus and consist of the small intestine (duodenum, jejunum and ileum) and the large intestine (colon and rectum). When something is wrong within this complex system, fecal incontinence (FI) may occur. FI is rarely due to one single factor and is, in fact, rather a symptom of underlying disease than a condition of its own.
FI is surprisingly common and affects men and women of all ages, but is most common among older people (who sometimes have to cope with urinary incontinence as well). As the condition may result from childbirth or obstetric trauma, more women than men are affected.
Underlying causes may be inflammatory bowel disease, intra-abdominal infection, colorectal cancer, and injury to the colon, rectum or anus. When treating mild FI, a simple adjustment of diet and/or medication is sometimes sufficient. Bowel and anal sphincter retraining is also used. For patients with severe FI, unresponsive to less invasive approaches, the end alternative is ostomy surgery – a procedure performed on millions of people worldwide.
Current treatments are not successful in the long-term and infections and other complications are common. The condition can be socially devastating and has a significant impact on the patients’ freedom of action and freedom of movement. Many patients feel ashamed and embarrassed, and fear of public humiliation may lead to social isolation. There is a need for development of new methods that can enable patients the freedom of movement and help them restore their dignity and self-esteem.
Many patients are reluctant to disclose incontinence, even when talking to their own physician. This reluctance can make it difficult to obtain accurate estimates of the true prevalence of FI. The estimated global prevalence ranges from 2% to 10%. One adult in every hundred has a regular problem (ICS, 2005). However, in the group of elderly people in residential care, prevalence of FI can be as high as 60% (Andramanakos, 2006).
Fig.2 (left) and Fig. 3 (right)

Many people suffering from fecal incontinence (FI) are too embarrassed to seek professional help, or they assume that nothing can be done. This is a pity, as there are ways to treat and manage the condition. However, current methods are seldom successful in the long-term and problems with infection, skin breakdown and other complications are common.
The first step, in the treatment of FI, is an individual assessment to determine the cause. This includes questions as to the history and pattern of the problem, related medical conditions and medications, diet and fluid intake. It is also important to ensure that there are no sinister symptoms, such as bleeding, anemia or unexplained weight loss, which might suggest bowel disease or even colon cancer (the second most common cancer in Western countries). Sometimes further tests are necessary, to image the anal sphincter muscles (by ultrasound or MRI), to inspect the lining of the bowel (endoscopy) or to test the nerve and muscle function of the lower bowel (anorectal testing). (International Continence Society, ICS, 2005)
Initially, most FI patients receive conservative therapy, including medical treatment and physiotherapy (i.e. electric stimulation and/or pelvic floor muscle training), which is successful for most patients with mild incontinence. These treatments can improve or restore bowel control or reduce the severity of fecal incontinence. However, the type of treatment depends on the cause and severity of the condition and more than one type of treatment may be necessary. Patients with severe symptoms should preferably be evaluated with endoscopy, and may eventually require surgery (Terra et al., 2005).
In the medical community, success of treatment is usually measured by the reduced frequency of episodes of incontinence. However, for the individual patient, the uncertainty of when an episode of incontinence may occur is the most important factor. It is that uncertainty that influences – and in some individuals may overwhelm – their daily life and sense of personal control (International Foundation for Functional Gastrointestinal Disorders, IFFGD, 2009).
It is common that the affected tries to hide the problem as long as possible, withdrawing from friends and family and often do not want to leave the house fearing possible public humiliation.
The socio economic burden of fecal incontinence (FI) surgery is substantial. A major problem for patients suffering from FI is the high risk of infection (50%), which prolongs the hospital stay and need for after care. If treated, without infection resources can be released and used within other areas of society, and the cost for medical care can be reduced.
FI has a dramatic impact on the health care system, as existing treatments are often complicated and associated with high costs. The cost of today’s commercially available artificial sphincters ranges from USD 6 400 to 16 000. This can be compared to the long-term cost of treatment of FI secondary to childbirth injury, estimated at more than USD 17 000 per patient (Person & Wexner, 2005).
Items with the strongest impact on the overall cost of FI are: incontinence material (diapers, pants, nappies, anal tampons, waterproof sheets, feces bags etc.), which accounts for a large part of total expenditures. For instance, in the US, FI accounts for more than USD 400 million per year for adult diapers only (Kalantar, Howell & Talley, 2002). In addition, it is the second leading cause of admission to long-term facilities in the US (Person & Wexner, 2005).
Furthermore, a large proportion of direct as well as indirect health care costs involved with FI, derive from the cleaning of incontinent patients. It has been estimated that personnel in charge of caring for incontinent patients who are permanently in institutions devote more than 13% of time available to this duty. However, the cost of health care personnel is not limited only to time and salary. Staff members who spend much of their time cleaning incontinent patients are more prone to dissatisfaction, depression and infection than are those engaged in other activities, and they are more likely to give up their jobs. (Ratto, Ponzi, Di Stasi & Parello, 2007)
Implantica is developing products with the aim to offer more effective treatments, facilitating for surgeons and patients, and thereby potentially reducing costs for hospitalization, medication and after care. Implantica’s new technological solutions, are designed with the intention to provide increased bowel control with fewer complications compared to conventional treatments.
Fecal incontinence is a problematic and often underestimated condition that affects a very large group of people. Besides associated health problems, it is socially devastating and embarrassing to live with lacking control of the bowel and its function, which leads to involuntary excretion and leaking. The existing treatment methods for fecal incontinence (FI) vary in success rate. Current treatments are not successful in the long-term and complications with infections are common. Developments of new methods that can give patients an improved quality of life are needed.
Implantica’s RectalRestore® is subject to further development and approval process and is not yet on the market. It isdesigned to control fecal incontinence, a treatment area lacking any optimal treatment today. This is intended to radically improve the patient’s quality of life.