Europe
RefluxStop™ is CE marked in Europe. It is currently available in:
- Germany
- United Kingdom
- Switzerland
- Spain
- Italy
- France
- Austria
- Sweden
- Norway
Prioritized Products
Gastrointestinal
Implantica’s AppetiteControl™ is subject to further development and approval process.
Today medication exists that has shown in larger studies to reduce body weight on average by approximately 10%. Ozempic, previously used for diabetes, and Wegovy, which was developed for obesity treatment and uses the same medical substance as Ozempic, have shown to cause increased weight loss by prolonging the stomach emptying time. These medications require a weekly injection, and the total weight loss is most suitable for low to mid-size obesity patients according to larger randomized trials performed1.
AppetiteControl™ is designed for more obese patients with BMI>40 or BMI >35 with co-morbidities or obese people preferring the risk profile of surgery compared to a life-long risk of the side effects of the medication. AppetiteControl™ is a device in our pipeline with a completely new treatment approach, designed to control appetite, and intended to avoid current surgeries’ debilitating and/or amputation-like procedures. When launched and integrated in our e-health platform, this device may support a possible paradigm shift in obesity surgery.
AppetiteControl™ is designed to support a desired weight level by achieving a feeling of fullness with less food intake. Patients could potentially be able to enjoy food intake and achieve full appetite with limited restrictions on what to eat.

AppetiteControl™ is an implant that is being designed to induce satiety, imitating the body’s own natural functions by stretching the upper part of the stomach in the same way as when the stomach becomes full of food. Patients are intended to be able to feel full after consuming an average portion of food. Preventing overeating will result in permanent weight loss.
AppetiteControl™’s main goal is for obese patients to not struggle with hunger. Healthy weight management is anticipated to be achieved where patients will feel hunger at mealtime and eat the amount that is necessary to maintain a certain weight without overeating. AppetiteControl™ is designed to imitate nature and stretch the upper part of the stomach wall to cause satiety when the programmed amount of food has been consumed.
The system is designed to include a food sensor to keep track of the patient’s eating. After the patient and doctor preferably together decide on the targeted weight, the aim is that the doctor at any time programs on distance how much the patient eats before the feeling of fullness is automatically activated for each meal by stretching the stomach wall thereby sending a signal of fullness to the brain. A patient’s weight should be decided by how much food intake occurs before fullness activation is made. If the patient eats a high caloric meal, the doctor programs less food intake. The doctor reviews his patients online perhaps every third month, checks the weight loss and adjusts how much the patient could eat to step by step achieve the targeted weight. No need for the patient to run to the hospital, everything will be designed to occur automatically. Patients should be able to have the flexibility to increase consumption for a special occasion.
AppetiteControl™ is designed to allow patients to enjoy food intake, eat what they want and still be able to maintain weight control. Affecting the appetite rather than physically stopping the food from passing is expected to provide higher quality of life while still losing weight.
The prevalence of obesity is large and growing dramatically, having more than doubled since 1990, with 2.5 billion overweight adults worldwide in 2022 and of those, more than 890 million obese (WHO 2022). The World Health Organization (WHO) defines obese as having a Body Mass Index (BMI) of greater than or equal to 30, calculated by dividing the weight in kilograms by the square of the height in meters.
From once having been considered a problem only in developed countries, overweight and obesity are now on the rise in low- and middle-income countries, particularly in urban settings. The rising epidemic reflects for the most part profound changes in society and in behavioral patterns: foods rich in fat, especially saturated fat, and sugar are readily available and generously consumed in a time when lifestyles are more and more sedentary.
Overweight and obesity can lead to many serious health consequences and sufferers have a shorter life expectancy. Depression and isolation are both common among obese and quality of life is affected by physical restrictions and by the negative image held by society. Many serious diseases can result from obesity including heart disease, diabetes, cancer, high blood pressure, infertility and acid reflux.
The Swedish Obese Subjects (SOS) study – a prospective controlled intervention study of bariatric surgery – is a significant research study involving 2,010 subjects that underwent bariatric surgery and 2,037 contemporaneously matched obese control subjects with a follow up period of up to 20 years. The SOS study results showed that bariatric surgery is associated with long-term weight loss and decreased overall mortality as well as a decreased incidence in many serious illnesses including diabetes, myocardial infarction, stroke and cancer1. The overall conclusion is that operating the obese people contributes to an overall societal reduction in expenditure.
Bariatric surgery refers to any surgical procedure on the stomach or intestines to induce weight loss. Today’s obesity surgical treatment methods include restrictive procedures, where the size of the stomach is reduced with a restricted outlet and, therefore, the amount of food that can be consumed is restricted, and malabsorptive procedures, where the stomach and the small intestines are removed, thereby changing the absorption of food and nutrition. The restrictive procedures do not change the absorption of food and nutrition, but they do restrict the amount of food that can be consumed. The two most common procedures are various gastric bypass procedures and gastric sleeve, however, these procedures fundamentally and irrevocably change the anatomy of the patients with a large portion of the stomach being removed. Vomiting is a common complication of these procedures.
A few examples are disclosed below.
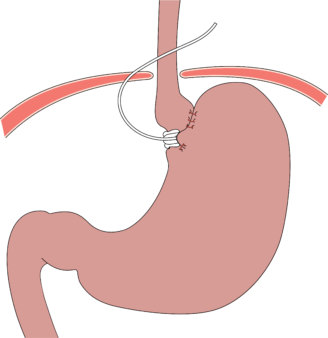
The Laparoscopic Adjustable Gastric Band is an example of a restrictive procedure, which involves wrapping a belt-like adjustable band around the upper portion of the stomach in order to decrease its size. The smaller upper part fills rapidly during food intake leading to a reduced capacity to eat and a feeling of satiety.
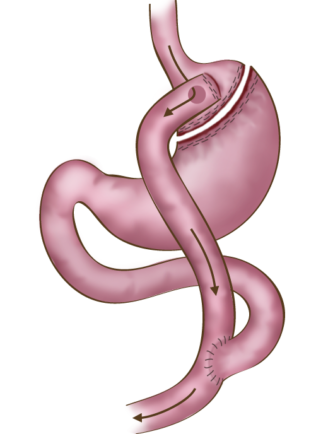
The most common forms of surgical treatments today include gastric bypass and sleeve gastrectomy. Gastric bypass involves removing a part of the stomach and the small intestine to restrict not only consumption but also absorption of food and nutrition. This surgical method is a restrictive procedure with a malabsorptive component. Gastric bypass procedures are invasive and involve changes in the anatomy, which has a large impact on the patient.
Sleeve gastrectomy is a surgical procedure for severely obese patients where approximately 80% of the stomach is removed. The stomach takes on the shape of a tube or sleeve and can hold much less food, thereby inducing weight loss by restricting food intake. One disadvantage is that acid reflux is surgically induced in up to 40% of sufferers.3,4
Intragastric balloons are used to treat less obese patients. The balloon is delivered down the esophagus and inflated in the stomach to reduce the amount of space inside the stomach. It can remain for up to six months before it erodes from gastric acid, and is therefore, not a long-term solution and not an alternative to bariatric surgery.
Bariatric surgery on severely obese patients is associated with long-term weight loss and decreased overall mortality. One of these studies involved 4,047 test subjects in two groups with an average of 10.9-year follow-up. The two most common causes of death were cancer and cardiovascular diseases, both were more frequent in the group that did not have bariatric surgery (Bengtsson, 2007). Weight loss also improves many obesity-associated conditions, such as diabetes.
As mentioned above, medication used for diabetes also stimulates weight loss. The diabetic medication Ozempic is most well-known, however, the same medication is approved for weight loss marketed under the trade name Wegovy. These medications have shown to be successful in treating low- to mid-size obese people with a weight loss between 5-15% of body weight. The side effects are well documented and not negligible, and treatment usually is life-long.
Overweight and obesity puts a massive cost burden on society today and it is constantly on the rise as the prevalence of these conditions increases worldwide.
As disclosed above, the Swedish Obese Subjects (SOS) study supports the overall conclusion that society saves a lot of money by operating the obese people.
Well over 890 million people are obese worldwide today and the numbers are constantly rising. Implantica is developing treatment solutions to improve the quality of life for the obese population.